Health Operator
Next: Personalised Health Assistant
Work happened and it took two months before I had time to focus on the substack again. But now there is for a change some time, so let’s goo….
Health Operator
Digitalisation means that services can be provided from anywhere in the world. Ubiquitousness of smart phones, good coverage in general everywhere, cheap cloud computing and miniturisation of technology opens up new possibilities to companies from anywhere in the world.
As examples, the customer can use their existing wearable or phone and with affordable add-on device and be offered real time diagnostics. Or as different example an autonomous vehicle or drone can deliver low-cost diagnostic devices or cheap diagnostics sticks for collecting samples, even in hard to reach places. User would use these to do i.e., nasal swab, or collect spit, sweat, tears and get either immediate results or use the drone to get the sample back for accurate analytics. If a health professional is on site, also blood samples can be taken for quick delivery. The measurements analysed by the service provider and recommended actions available almost immediately.
This allows to operate health diagnostics and motivational services on global scale from anywhere. Some local co-operation partners is often needed for example as some samples require local lab analytics.
For a remote diagnostics provider focus is important as they want to differentiate. A single company can specialise in just one disease – say diabetes and offer comprehensive care package around it. Such a service might contain continuous monitoring of vital signals relevant for the disease, real time analytics based on measurement, actions and recommendations when something is not fine – for example alerts or automated calling of ambulance in emergency and gamified challenges to improve health and cope with the disease better. Chatbots always available for helping you with your disease, online consultations with specialists when needed, online learning packages containing detailed information on the condition, online forums and face to face meetups for peer to peer help and discussions.
The services would be provided from remove via the health cloud.
Being narrowly focused and operating in many countries (like EU or globally) allows the company to accumulate learning. For the patient the value proposition will be: “Select the world’s best company for treating your disease who take care of millions of patients daily with your condition rather than a generalist, who also be good but not as good as we”.
Economics of scale also mean that this company can invest much more into the treatment of a single disease and still provide the services at cheaper rate.
This is the health operator.
Most interaction would be through the digital tools, with additional sensors or one-time disposable analysis stickers. Combined with data from health data records to improve accuracy of remote analytics, if user and local legislation allows. This all in near real time around the clock on every day. Test requiring very high reliability would still be made in local laboratories that the health operator has a contract with. The global operator may have own doctors or contracts with local health providers (public or private) for physical consultations.
In order to help people to select their health operator, the reputations need to be public. Reputation has two parts – measured quality in terms of effectiveness and perceived quality – how humanly the patients felt they were treated by a particular provider.
Compared with current mode where when something happens at 1AM and having to endure the long wait until morning, through weekend or several weeks (read: months) for non-urgent, this is quite an improvement.
As citizen I might select one health operator to treat my high blood sugar, another for my blood pressure and third one for back pains and the rest of the health would be provided by the local default health provider. As long as all see interventions and impact of each other through the health records or can consult each other using standardised practices, they can work together.
For people who do not yet have a chronic disease, the health operator would offer a wider service selection containing general health data monitoring, analytics and motivational services to help people reach their targets through various challenges and other gamified activities, online courses on health, health assistants, online consultations etc. Different packages for different customers like people living alone in remote areas, someone taking care of an elderly relative or a child with a disability, people doing extreme sports, active pensioners etc.
Especially attractive for employees, who know the cost when staff get sick and company cannot deliver on its promises (both direct costs and loss of customers).
So, nothing prevents mixing and matching public and private services once data and services are accessible via an open API. Opening the API would follow similar principles as applied for financial services with the PSD2 directive in Europe.
People could start with a private health operator first with all kinds of self-test, cloud analytics and interventions, then go to a public lab for tests and finally to a doctor appointment at public health center with the information collected following all the time. The health chain is seamless.
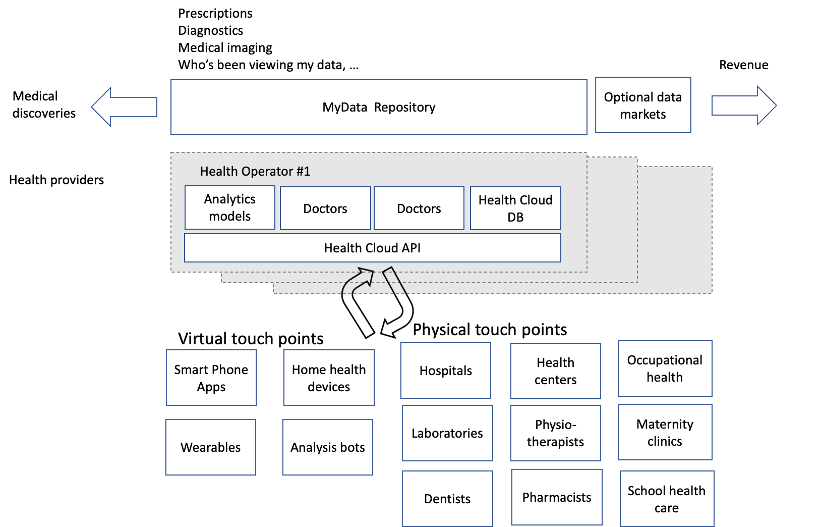
The image below shows overview of this:
Heck, even public side could digitalise, move to a 24*7 model and become a health operator with massive savings to society.
Building Remote Care Iteratively
As described on previous post, building this type of automated remote support is best done iteratively. For example so that in the beginning all requests are handled by human experts. I.e., medical professionals do all the diagnostics using existing tools like video calls, image analytics, lab results and their own experience.
This starts building a data set of common issues and solutions that in time are used to build models to suggest diagnostics. Going from easy issues first to more complex over time. Always working so that when the models are unsure whether they have the right answer (when they have low score in probability) the questions are forwarded to a human expert, who provides the answer manually. And in all cases making available to experts how sure the model thinks it is and what other alternatives can be considered. This keeps experts in control.
Personal Health Budget
One worry is that market moves towards just a few global service providers and tax payers (or other parties carrying the costs like enterprises) lose understanding what the real costs are. Monopolies or oligopolies have very little need to innovate and improve.
This can be mitigated if patients have the means to participate into organising health provision. For example with their personal health budgets. This would be a certain monetary sum out of their taxes that they can pool to run small scale competing services or fund experiments. A concept similar to Citizen’s Automation Budget presented earlier.
Why would this be useful? Let’s take an example. Today people with difficulties walking often get a wheelchair which makes moving difficult in much of the world around us. In addition, you cannot speak eye to eye from a wheelchair but everyone talks down to you.
There is a set of small companies developing exoskeletons. Exoskeletons are lightweight structures with power source that help or replace the function of limbs. In essence allowing people to stand up and walk when they have severely impaired or lost that ability.
They allows people much greater freedom of movement. However, the current health system is reluctant to try them out. The companies developing them are small startups that health system is not aware, they are not part of the official approved treatment standards and there is no culture of trying out completely novel systems. Health organisations purchase products that are tested and brought to market by big vendors that they feel comfortable buying from.
With personal health budget patient associations could organise the pooling of resources so that active patients could try out different types of new, upcoming treatments and solutions. If they succeed, the health system could then officially become aware of them and could starting thinking into taking them into the portfolio of available solutions.
One potential occupation in future could be finding out effective, upcoming solutions from anywhere. Looking for cost-efficient and effective ways to prevent or treat health conditions not yet in active use in own country and helping to start experiments with health budgets to validate them. By introducing them, one could earn a certain percentage of the proven savings, once the savings start coming in.
A different use case where health budgets seem like a good fit, is the study of old, existing medicine that are no longer under license (patent no longer valid). Commercial pharmaceutical companies have no interest in studying if some old and safe medicine might be good to treat a different disease. These off-license medicine are made en-mass and only cost a penny and medical studies tend to be very expensive. Health budget concept to the rescue.
Likewise there is very low interest to study scientifically herbal medicines used for hundreds of years. Lions mane is one example that has raised some interest lately to slow down aging, regulate blood sugar, high blood pressure etc. Since it has low or no commercial value, it’s currently understudied.
Third direction is to look for one-time solutions to health issues. For commercial companies any treatment that lasts a life-time is ideal from income perspective. One-shot solutions can destroy many such opportunities. However these also have big income potential and medical companies are active in such research, but health budgets could speed up development or find parallel solutions that get released into open without expensive licenses.
As examples there are for example vaccines against different cancers under development. These work on the principle that cancer cells have molecules that healthy cells do not have. Vaccines can be used to tell the immune system to identify these proteins. When cancer cells later in life develop, the immune system can recognise and destroy them.
Health budgets are an improvement but not a complete solutions. There is a dilemma here as ideally there is a bigger reward for preventive solutions than treating existing conditions. Prevention carries a much bigger saving, but calculating difference is often impossible or at least difficult. Estimating impact of something that did not happen remains difficult.
Examples of Health Operator Services
Let’s roll a few ideas what the health operator could offer in addition to consultation, diagnosis and life coaching (eating habits, sleep, exercise motivation).
There are in no particular order.
Cloud Rehabilitation
Traditional rehabilitation is based on a one-to-one interaction between therapist and patient. This is very effective but carries high costs. Due to costs and availability of therapists, patients don’t have access to the ideal number of hours of treatments, nor the required intensity.
A much cheaper alternative is to give inexpensive motion trackers to patients and have an application motivate and track as they exercise. This way the remote health team can track how the patients rehabilitate themselves. Analytics can be developed to try out and improve exercise programs and find out better ways to motivate different types of personalities.
Enterprise Services
Various health problems are big ticket items for enterprises of all sizes and mental problems (depression, not feeling motivated, fatigue due to lack of sleep, self-medication with alcohol) are a major contributor to them.
For companies the health operator can offer a comprehensive life coach package in similar manner than we envisioned to be offered to unemployed people in Public Service Example post (F1 support model towards the end). Clarifying what they truly want from life and then going through the current medical and mental state, how to maintain physical condition and prevent diseases (exercise, rest, sleep, healthy food).
In a bigger organisation the payment could be directly from savings accrued as they are relatively easy to see. In smaller some simple monthly price etc.
Therapy Robots
Different therapy and care robots have been measured to relax and soothe people and provide additional opportunities for interaction when people can nurture them, and their surface has been made soft and animal fur like, so it feels good to pet them and they respond.
Therapy robots can also have voice interfaces and answer questions and provide a listening ear. Voice enabled therapy robots are especially helpful to people who suffer from dementia and are feeling loneliness when they no longer can remember everything. Normal people get annoyed when the discussion returns over and over to the same topic, but robots can endlessly discuss any topic, even old ones.
At the same time, these robots can passively monitor the environment and for example analyze gases emitting from healing wounds and relay it back, telling effectively how well the patient is recovering.
Robots at home can also help in daily chores to dispense mediation, bring food and put it in microwave, feed if having problems holding utensils, clean around and assist in to toilet and walk around the house.
Robots for Hospitals
Health operator can also offer services to hospitals, not just individuals.
In hospitals a lot of the work is indirect, and logistics especially has big part. These tasks are for example lifting patients, moving them from place to place or helping them move self, fetching medical supplies like samples, medicine, linen, meals and documenting all work. They all can be automatized with care robots releasing quite a bit of time to direct interaction with patients.
Some direct work can also be automatized. Already now there are robots that helps bedridden patients wash themselves – a big improvement in privacy.
In Finland it is estimated that at least 20 percent of current work of registered nurses and practical could be replaced with robotics and existing automations giving one extra day of direct patient work per week to each one. As the population is getting older, the total amount of work as such is unlikely to reduce in hospitals even when a growing part will be automatised.
Exoskeletons
Moving around with wheel chairs or rollators is difficult as the built and natural environments are mostly made or suitable for walking. Exoskeletons were already mentioned as a solution.
There are many ways to build wearable harnesses and they can be controlled
with either hands or by reading from the nerves or muscles of the patient the signals how to move. Some solutions only provide assistive force if the patient still has some power in muscles – this allows to retain the ability; others are true self-walking harnesses.
There is a big imbalance as society spends a lot to construct accessibility features into buildings and apartments but very little into recovering ability to walk with new types of assistive devices. This may change. The weakest person becoming the tallest, fastest and strongest one.
Exoskeletons also have uses outside of health in allowing workers to lift very heavy weights and work long without getting tired.
https://en.wikipedia.org/wiki/Robot_leg
Obstacles
The biggest obstacles to the health operator model are regulatory. Health like practically all verticals suffers from regulatory capture. Valid concerns about patient health and privacy are also enormously powerful tools in protecting the status quo.
Some solutions to this could be the above scetched Health Budget model and the Be Your Own Mouse concept from previous post.